Transcript
ReachMD Announcer:
You’re listening to Project Oncology on ReachMD. This Medical Industry Feature, titled “An Approach to Treating BPDCN Patients with Prior or Concomitant Hematologic Malignancies,” is sponsored by Stemline Therapeutics, Inc., a Menarini Group Company. Here’s your host, Dr. Charles Turck.
Dr. Turck:
Welcome to Project Oncology on ReachMD. I’m Dr. Charles Turck, and here with me to discuss the long-term findings on a treatment option for patients with hematologic malignancies and blastic plasmacytoid dendritic cell neoplasm, or BPDCN for short, is Dr. James McCloskey. Dr. McCloskey currently leads the Division of Leukemia as the interim Chief at Hackensack University Medical Center and Jersey Shore University Medical Center at Hackensack Meridian Health, and is a paid consultant for Stemline Therapeutics. Dr. McCloskey, welcome to the program.
Dr. McCloskey:
Thank you for having me, it’s great to be here.
Dr. Turck:
To start us off, Dr. McCloskey, can you give us some background on BPDCN? Because as I understand it, other malignancies are often associated with it, is that correct?
Dr. McCloskey:
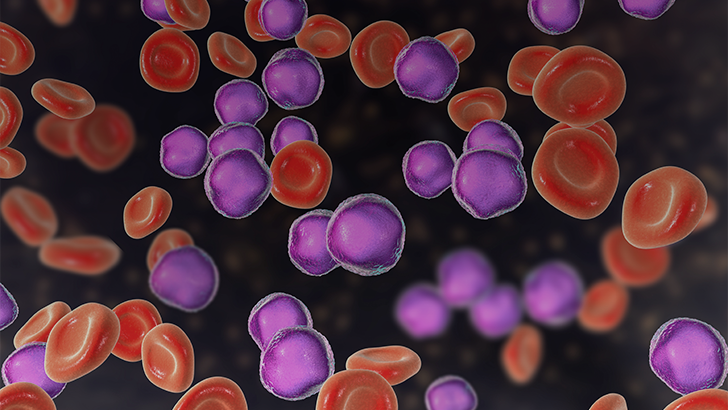
Yes, that’s absolutely right, but before we dive into that, it’s important to know that BPDCN is a highly aggressive myeloid malignancy. It originates from precursors of plasmacytoid dendritic cells and is characterized by the overexpression of CD123, which is also known as interleukin-3 receptor alpha.1 Now as you alluded to, approximately 10 to 20% of BPDCN patients have prior or concomitant hematologic malignancies, which are often referred to as PCHM. These can include myelodysplastic syndrome, chronic myelomonocytic leukemia, chronic myeloid leukemia, and acute myeloid leukemia, among others—all of which can worsen their prognosis.1
The presence of these prior or concomitant malignancies really highlights the importance of reaching an accurate diagnosis and the regular monitoring for cytopenia.1 Additionally, patients with PCHM may have a unique disease biology that affects their response to therapy.1
Dr. Turck:
With that background in mind, let’s zero in on treatment. What options are currently available?
Dr. McCloskey:
Well currently, TAGRAXOFUSP, also known as ELZONRIS, is a CD123-directed cytotoxin indicated for the treatment of BPDCN in adults and in pediatric patients two years and older. It’s the first and only CD123-directed therapy approved by the US FDA and the European Medicines Agency for BPDCN treatment after a pivotal, nonrandomized, multistage, phase one/two, open-label, multicenter evaluation of TAGRAXOFUSP as a monotherapy.1 The preliminary analysis of the data consisted of 40 patients with BPDCN that were treated with TAGRAXOFUSP. Of these patients, 22 were treated in the first-line setting while 18 were treated in the relapsed or refractory treatment arm. Regardless of previous treatment, TAGRAXOFUSP resulted in a 75% overall response rate in first-line patients, with a median response duration of 25 months for patients achieving complete response or complete response with residual skin abnormalities. And 57% achieved complete response plus complete response with residual abnormality not indicative of active disease, which is also referred to as CRc.2 Finally, 51% of treatment-naïve patients achieving complete responses plus CRc were able to undergo hematopoietic stem cell transplants for further treatment,2 and TAGRAXOFUSP also demonstrated a well-characterized safety profile with a defined management strategy for capillary leak syndrome, or CLS.2
So those were the preliminary results, and the report we’re going to be talking about today focuses on a subgroup analysis of this pivotal trial. Specifically, it evaluated the efficacy and safety of TAGRAXOFUSP in eight treatment-naïve patients with PCHM.
ReachMD Announcer:
For more information on TAGRAXOFUSP, please see full Prescribing Information, including the Boxed WARNING, at ELZONRIS.com/hcp.
Boxed WARNING: CAPILLARY LEAK SYNDROME
- Capillary Leak Syndrome (CLS), which may be life-threatening or fatal , can occur in patients receiving ELZONRIS. Monitor for signs and symptoms of CLS and take actions as recommended.
Dr. Turck:
So then let’s dive into that report, Dr. McCloskey. What can you tell us about the study design?
Dr. McCloskey:
This was a sub analysis of a multi-center, four-stage, single-arm, phase one/two trial that evaluated the use of TAGRAXOFUSP as a monotherapy for newly diagnosed or relapsed or refractory BPDCN.1 Of the 65 first-line patients included in the pivotal trial, this sub analysis looked at a cohort of eight patients with at least one PCHM as I mentioned before. The trial was conducted in four stages. In the first stage, TAGRAXOFUSP was initiated at 7 or 12 micrograms per kilogram, and for the remainder of the stages, it was administered at the 12 microgram per kilogram dose.1 TAGRAXOFUSP was administered via IV infusion on days one through five of a 21-day-cycle.1 It should be noted that the dosing period may be extended for dose delays up to day 10 of each cycle.3 The primary clinical endpoints were overall survival, overall response rate, and complete response plus CRc.1
Dr. Turck:
And what were the characteristics of patients who were eligible for this study?
Dr. McCloskey:
Patients who were 18 years or older were eligible if they had a diagnosis of BPDCN according to the WHO classification or confirmed by hematopathology. This distinction was important because histological and/or cytological evidence of BPDCN was needed to measure treatment response compared to baseline. Patients also needed to have an Eastern Cooperative Oncology Group performance status ranging between 0 and 2, which means that patients were restricted in work activity but were ambulatory and capable of self-care. Patients who had cancer within 2 years of enrollment, with substantial potential for recurrence and/or ongoing active malignancy, could be included following a discussion with the sponsor. And finally, patients with adequate cardiac, renal, and hepatic function in addition to an albumin level greater than or equal to 3.2 grams per deciliter and normal left ventricular ejection fraction at baseline were also eligible.1
Dr. Turck:
As a quick follow-up to that, Dr. McCloskey, can you tell us about the participants who enrolled in this study?
Dr. McCloskey:
Absolutely. So in all, 65 treatment-naïve patients were eligible for inclusion. Of these, eight patients had PCHM, and one patient even had two.1 Those reported PCHM included myelodysplastic syndrome, polycythemia vera, chronic myelomonocytic leukemia and myelodysplastic syndrome, plasma cell myeloma, Hodgkin’s disease, and lymphoma.1
The average age of patients in this subgroup was approximately 68, and 75% of patients were male. Lastly, time from PCHM diagnosis to the BPDCN diagnosis ranged between 4 and 14 years.1
Dr. Turck:
For those just tuning in, you’re listening to Project Oncology on ReachMD. I’m Dr. Charles Turck, and today I’m speaking with Dr. James McCloskey about the effects of TAGRAXOFUSP in patients with BPDCN and prior or concomitant hematologic malignancies.
So Dr. McCloskey, now that we know more about the patients who were involved in this subgroup analysis, let’s turn our attention to the key findings. First, what were the results regarding the safety profile of TAGRAXOFUSP and its adverse effects?
Dr. McCloskey:
So the most common adverse effects occurring with an incidence of greater than or equal to 20% in either patient cohort were increased ALT, AST, hypoalbuminemia, thrombocytopenia, pyrexia, weight gain, and nausea.1 CLS is a risk,1 which may be life-threatening or fatal, and it’s the basis for the boxed warning.3 The safety profile in patients with PCHM was consistent with the entire study population and no new safety findings were observed in this population.1
Dr. Turck:
Great. And what can you tell us about the findings on the efficacy of TAGRAXOFUSP?
Dr. McCloskey:
Similar rates of complete response plus CRc were seen across patients with and without PCHM—50% and 58%, respectively. And overall response rate was also similar for patients with and without PCHM—88% and 74%, respectively.1
18 patients with no history of PCHM were bridged to hematopoietic stem cell transplant after achieving a CRc that was not indicative of active disease. However, one patient who did have a history of a PCHM was also bridged to transplant.1
And the last key finding I’d like to share is that the median overall survival was significantly longer at 18.9 months in patients without a history of PCHM compared to 6.3 months in patients who had that kind of history.1 This is in keeping with patients with PCHM historically having poorer prognoses than those without PCHM.1
Dr. Turck:
Now we’re almost out of time for today, Dr. McCloskey, so before we close, are there any final thoughts you’d like to share with our listeners?
Dr. McCloskey:
Sure, so just to recap, today we reviewed the long-term data for the only FDA-approved first-line and relapsed or refractory treatment for patients with BPDCN who also presented with a PCHM, which is consistent with previous reports.1 Also consistent with previous reports were the response rates as compared to patients without a PCHM after receiving treatment with TAGRAXOFUSP, but this was also accompanied by a lower median overall survival.1 Despite the presence of PCHM, approximately 50% of these patients, including eight patients who had at least one PCHM, achieved a complete response and/or a complete response with residual skin abnormality not indicative of active disease.1 And while these patients were heterogenous in terms of the type and duration of prior malignancies as well as treatment histories—which are all factors that could worsen prognosis and treatment outcomes—TAGRAXOFUSP demonstrated efficacy in this patient population.1
Dr. Turck:
Thank you, Dr. McCloskey, that was a great way to sum up our discussion today. And as that brings us to the end of our program, I’d like to thank my guest, Dr. James McCloskey, for speaking with us about the safety and efficacy data from a subgroup analysis focusing on the treatment option TAGRAXOFUSP. Dr. McCloskey, it was great speaking with you!
Dr. McCloskey:
You as well, Dr. Turck, thank you.
Dr. Turck:
For ReachMD, I’m Dr. Charles Turck. Please listen to the following Important Safety Information, including the Boxed WARNING.
ReachMD Announcer:
INDICATION
- ELZONRIS is a CD123-directed cytotoxin indicated for the treatment of blastic plasmacytoid dendritic cell neoplasm (BPDCN) in adults and in pediatric patients 2 years and older.
IMPORTANT SAFETY INFORMATION
Boxed WARNING: CAPILLARY LEAK SYNDROME
- Capillary Leak Syndrome (CLS) which may be life-threatening or fatal, can occur in patients receiving ELZONRIS. Monitor for signs and symptoms of CLS and take actions as recommended.
WARNINGS AND PRECAUTIONS
Capillary Leak Syndrome
- Capillary leak syndrome (CLS), including life-threatening and fatal cases, has been reported among patients treated with ELZONRIS. In patients receiving ELZONRIS in clinical trials, the overall incidence of CLS was 53% (65/122) patients, including Grade 1 or 2 in 43% (52/122) patients, Grade 3 in 7% (8/122) patients, Grade 4 in 1% (1/122) patients, and four fatalities (3%). The median time to onset was 4 days (range - 1 to 46 days), and all but 5 patients experienced an event in Cycle 1.
- Before initiating therapy with ELZONRIS, ensure that the patient has adequate cardiac function and serum albumin is greater than or equal to 3.2 g/dL. During treatment with ELZONRIS, monitor serum albumin levels prior to the initiation of each dose of ELZONRIS and as indicated clinically thereafter, and assess patients for other signs or symptoms of CLS, including weight gain, new onset or worsening edema, including pulmonary edema, hypotension or hemodynamic instability.
Hypersensitivity Reactions
- ELZONRIS can cause severe hypersensitivity reactions. In patients receiving ELZONRIS in clinical trials, hypersensitivity reactions were reported in 43% (53/122) patients treated with ELZONRIS and were Grade ≥ 3 in 7% (9/122) patients. Manifestations of hypersensitivity reported in ≥ 5% of patients include rash, pruritus, and stomatitis. Monitor patients for hypersensitivity reactions during treatment with ELZONRIS. Interrupt ELZONRIS infusion and provide supportive care as needed if a hypersensitivity reaction should occur.
Hepatotoxicity
- Treatment with ELZONRIS was associated with elevations in liver enzymes. In patients receiving ELZONRIS in clinical trials, elevations in ALT occurred in 79% (96/122) patients and elevations in AST occurred in 76% (93/122) patients. Grade 3 ALT elevations were reported in 26% (32/122) patients. Grade 3 AST elevations were reported in 30% (36/122) patients and Grade 4 AST elevations were reported in 3% (4/122) patients. Elevated liver enzymes occurred in the majority of patients in Cycle 1 and were reversible following dose interruption.
- Monitor alanine aminotransferase (ALT) and aspartate aminotransferase (AST) prior to each infusion with ELZONRIS. Withhold ELZONRIS temporarily if the transaminases rise to greater than 5 times the upper limit of normal and resume treatment upon normalization or when resolved.
ADVERSE REACTIONS:
Most common adverse reactions (incidence ≥ 30%) are capillary leak syndrome, nausea, fatigue, pyrexia, peripheral edema, and weight increase. Most common laboratory abnormalities (incidence ≥ 50%) are decreases in albumin, platelets, hemoglobin, calcium, and sodium, and increases in glucose, ALT and AST.
Please see full Prescribing Information, including the Boxed WARNING.
To report SUSPECTED ADVERSE REACTIONS, contact Stemline Therapeutics, Inc. at 1-877-332-7961 or contact the FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
ReachMD Announcer:
This program is brought to you by Stemline, a Menarini Group company. If you missed any part of this program, visit Project Oncology on ReachMD.com, where you can Be Part of the Knowledge.
REFERENCES
- Pemmaraju N, et al. Tagraxofusp, a CD123-directed therapy, in patients with blastic plasmacytoid dendritic cell neoplasm and prior or concomitant hematologic malignancies: subgroup analysis of a pivotal trial. Poster presented at: 65th ASH Annual Meeting & Exposition. December 10-13, 2022: New Orleans, LA.
- Pemmaraju N, Sweet KL, Stein AS, et al. Long-Term Benefits of Tagraxofusp for Patients With Blastic Plasmacytoid Dendritic Cell Neoplasm. J Clin Oncol. 2022;40(26):3032-3036. doi:10.1200/JCO.22.00034
- ELZONRIS (tagraxofusp-erzs) [prescribing information]. New York, NY: Stemline Therapeutics; 2018.
MAT-US-TAG-00025 / Copyright 2023- Stemline Therapeutics, Inc.
All rights reserved. 12/2023