Announcer:
You're listening to The Drug Report on ReachMD, hosted by Linda Bernstein, Pharm.D., Clinical Professor on the Volunteer Faculty of the School of Pharmacy, University of California, San Francisco.
Dr. Bernstein:
Welcome to The Drug Report with a special focus on the COVID-19 pandemic.
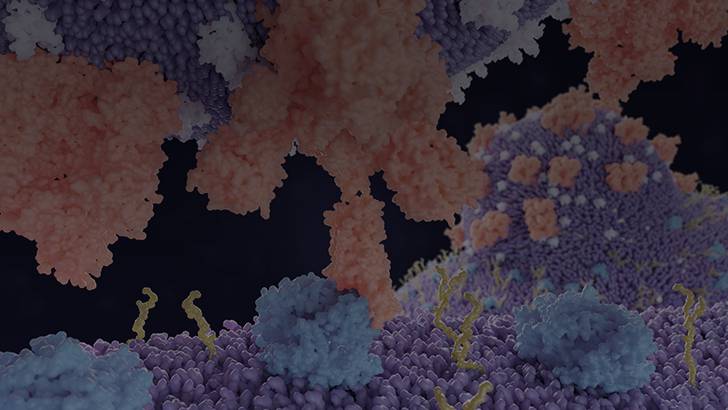
A recent article published in the New England Journal of Medicine discussed the relationship between the renin-angiotensin-aldosterone system (RAAS) and recent coronaviruses including the SARS-CoV-1, responsible for the 2002 to 2004 SARS epidemics and SARS-CoV-2, the source of the current COVID-19 pandemic. The authors, headed by Muthiah Vaduganathan, M.D., M.P.H., describe the RAAS as an “elegant cascade of vasoactive peptides that orchestrate key processes in human physiology.” The virus interfaces with the RAAS through angiotensin-converting enzyme 2 (ACE2), an enzyme that physiologically counters RAAS activation, but also serves as a receptor for both SARS viruses. The SARS virus, ACE2 interaction, has been proposed as a potential factor in viral infectivity and there are concerns that RAAS inhibitors may alter ACE2 such that it may be in part responsible for the virulence of the disease in the ongoing pandemic. This view as expressed by some media sources has resulted in requests by some health systems for discontinuation of ACE inhibitors and angiotensin-receptor blockers (ARBs) both for prophylaxis and in the context of suspected COVID-19.
The authors state that there is an urgent need for guidance in the use of these drugs in COVID-19 patients because ACE inhibitors and ARBs are commonly used worldwide.
Select preclinical studies have suggested that RAAS inhibitors may increase ACE2 expression, raising concerns regarding their safety in patients with COVID-19. Insufficient data are available to determine whether these observations readily translate to humans, and no studies have evaluated the effects of RAAS inhibitors in COVID-19, although numerous clinical trials are in the works.
The authors stated that the data in humans is currently too limited to support or refute these hypotheses and concerns due to the uncertain effects of RAAS blockers on ACE2 levels and activity in humans. They propose an alternative hypothesis that ACE2 may actually be beneficial rather than detrimental to patients with COVID-19 lung injury. They feel withdrawal of RAAS inhibitors may be harmful in certain high-risk patients with known or suspected COVID-19.
Given the available evidence, the authors and multiple specialty medical societies believe that despite theoretical concerns and uncertainty pertaining to the effect of RAAS inhibitors on ACE2 and its potential relationship to COVID-19 severity, RAAS inhibitors should be continued in patients who are otherwise in stable condition who are at risk for or are being evaluated for COVID-19. Additional data from ongoing and upcoming clinical trials may inform otherwise in the future, but clinicians need to be aware of the unintended consequences of prematurely discontinuing proven therapies in “response to hypothetical concerns that may be based upon incomplete experimental evidence.” Abrupt withdrawal of RAAS inhibitors in high-risk patients, including those who have heart failure or have had myocardial infarction, may result in clinical instability and adverse health outcomes. For more information on clinical trials associated with RAAS Inhibitors in Patients with COVID-19, see clinicaltrials.gov.
For The Drug Report, I’m pharmacist, Dr. Linda Bernstein
Announcer:
To access this episode and others from The Drug Report, visit ReachMD.com/drugreport, where you can be part of the knowledge. Thanks for listening.

Facebook Comments