ReachMD
Be part of the knowledge.™Use of RAS antagonists and mortality in HF
Literature - Lund LH et al. JAMA. 2012;308:2108-17.
JAMA. 2012;308:2108-17. doi: 10.1001/jama.2012.14785.
A prospective study included data on 41,791 patients in the Swedish Heart Failure Registry who were registered at 64 hospitals and 84 outpatient clinics from 2000 to 2011. Of these, 16,216 patients with HFPEF were treated with RAS antagonists (n=12,543) or not treated (n=3,673). The mean age of the patients was 75 years and 46% were women.
1. Steinberg BA, Zhao X, Heidenreich PA, et al; Get With the Guidelines Scientific Advisory Committee and Investigators. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation. 2012;126(1):65-75.
2. Yusuf S, Pfeffer MA, Swedberg K, et al; CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet. 2003;362(9386):777-781.
3. Cleland JG, Tendera M, Adamus J, et al; PEP-CHF Investigators. The perindopril in elderly people with chronic heart failure (PEPCHF) study. Eur Heart J. 2006;27(19):2338-2345.
4. Massie BM, Carson PE, McMurray JJ, et al; IPRESERVE Investigators. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359(23):2456-2467.
5. McMurray J. Renin angiotensin blockade in heart failure with preserved ejection fraction: the signal gets stronger. Eur Heart J. 2006;27(19):2257-2259.
Context:
Heart failure with preserved ejection fraction (HFPEF) may be as common and as lethal as heart failure with reduced ejection fraction (HFREF). Three randomized trials of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (ie, renin-angiotensin system [RAS] antagonists) did not reach primary end points but may have had selection bias or been underpowered.
Objective:
To test the hypothesis that use of RAS antagonists is associated with reduced all-cause mortality in an unselected population with HFPEF.
Design, setting, and patients:
Prospective study using the Swedish Heart Failure Registry of 41,791 unique patients registered from 64 hospitals and 84 outpatient clinics between 2000 and 2011. Of these, 16,216 patients with HFPEF (ejection fraction ≥40%; mean [SD] age, 75 [11] years; 46% women) were either treated (n = 12,543) or not treated (n = 3673) with RAS antagonists. Propensity scores for RAS antagonist use were derived from 43 variables. The association between use of RAS antagonists and all-cause mortality was assessed in a cohort matched 1:1 based on age and propensity score and in the overall cohort with adjustment for propensity score as a continuous covariate. To assess consistency, separate age and propensity score-matched analyses were performed according to RAS antagonist dose in patients with HFPEF and in 20,111 patients with HFREF (ejection fraction <40%) in the same registry.
Main outcome measure:
All-cause mortality.
Results:
In the matched HFPEF cohort, 1-year survival was 77% (95% CI, 75%-78%) for treated patients vs 72% (95% CI, 70%-73%) for untreated patients, with a hazard ratio (HR) of 0.91 (95% CI, 0.85-0.98; P = .008). In the overall HFPEF cohort, crude 1-year survival was 86% (95% CI, 86%-87%) for treated patients vs 69% (95% CI, 68%-71%) for untreated patients, with a propensity score-adjusted HR of 0.90 (95% CI, 0.85-0.96; P = .001). In the HFPEF dose analysis, the HR was 0.85 (95% CI, 0.78-0.83) for 50% or greater of target dose vs no treatment (P < .001) and 0.94 (95% CI, 0.87-1.02) for less than 50% of target dose vs no treatment (P = .14). In the age and propensity score-matched HFREF analysis, the HR was 0.80 (95% CI, 0.74-0.86; P < .001).
Conclusion:
Among patients with heart failure and preserved ejection fraction, the use of RAS antagonists was associated with lower all-cause mortality.
Association between use of renin-angiotensin system antagonists and mortality in patients with heart failure and preserved ejection fraction.
Lund LH, Benson L, Dahlström U, Edner M.JAMA. 2012;308:2108-17. doi: 10.1001/jama.2012.14785.
Background
About half of patients with heart failure have heart failure with preserved ejection fraction (HFPEF) or diastolic heart failure. Mortality can be as high as in heart failure with reduced ejection fraction (HFREF) [1]. In 3 randomized controlled trials, RAS antagonists did not improve primary outcomes in HFPEF, although there were benefits in primary and secondary outcomes [2-4]. These trials may have had selection bias or insufficient power [5]. This study evaluated whether the use of RAS antagonists is associated with reduced all-cause mortality in an unselected population with HFPEF.A prospective study included data on 41,791 patients in the Swedish Heart Failure Registry who were registered at 64 hospitals and 84 outpatient clinics from 2000 to 2011. Of these, 16,216 patients with HFPEF were treated with RAS antagonists (n=12,543) or not treated (n=3,673). The mean age of the patients was 75 years and 46% were women.
Main results
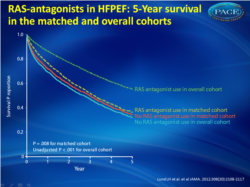
- Overall, crude 1-year survival was 86% for patients with HFPEF treated with RAS antagonists vs. 69% for patients not treated (propensity score-adjusted HR=0.9; 95% CI, 0.85-0.96). Five-year survival was 55% vs. 32%, respectively (fig. 1).
- In the matched cohort, 1-year survival was 77% for patients treated with RAS antagonists vs. 72% for patients not treated (HR=0.91; 95% CI, 0.85-0.98). Five-year survival was 36% vs. 34%, respectively.
- In the HFPEF dose analysis, 1-year survival was 80% for low-dose RAS antagonist treatment, 82% for high dose and 76% for no treatment. Five-year survival was 39%, 43% and 40%, respectively.
- A HR of 0.85 (95% CI, 0.78-0.83) was calculated for high-dose treatment vs. no treatment and 0.94 (95% CI, 0.87-1.02) for low-dose treatment vs. no treatment.
- Analysis of propensity for treatment-matched patients with HFREF, 1-year survival was 67% for patients treated with RAS antagonists vs. 58% for patients not treated; 5-year survival was 29% vs. 23%, respectively.
Conclusion
Use of RAS antagonists was associated with reduced all-cause mortality in a broad unselected population of patients with HFPEF. These results together with the signal toward benefit in randomized controlled trials suggest that RAS antagonists may be beneficial in patients with HFPEF, but this should be confirmed in an appropriately powered randomized trial.
References
1. Steinberg BA, Zhao X, Heidenreich PA, et al; Get With the Guidelines Scientific Advisory Committee and Investigators. Trends in patients hospitalized with heart failure and preserved left ventricular ejection fraction: prevalence, therapies, and outcomes. Circulation. 2012;126(1):65-75.2. Yusuf S, Pfeffer MA, Swedberg K, et al; CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet. 2003;362(9386):777-781.
3. Cleland JG, Tendera M, Adamus J, et al; PEP-CHF Investigators. The perindopril in elderly people with chronic heart failure (PEPCHF) study. Eur Heart J. 2006;27(19):2338-2345.
4. Massie BM, Carson PE, McMurray JJ, et al; IPRESERVE Investigators. Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med. 2008;359(23):2456-2467.
5. McMurray J. Renin angiotensin blockade in heart failure with preserved ejection fraction: the signal gets stronger. Eur Heart J. 2006;27(19):2257-2259.
Context:
Heart failure with preserved ejection fraction (HFPEF) may be as common and as lethal as heart failure with reduced ejection fraction (HFREF). Three randomized trials of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (ie, renin-angiotensin system [RAS] antagonists) did not reach primary end points but may have had selection bias or been underpowered.
Objective:
To test the hypothesis that use of RAS antagonists is associated with reduced all-cause mortality in an unselected population with HFPEF.
Design, setting, and patients:
Prospective study using the Swedish Heart Failure Registry of 41,791 unique patients registered from 64 hospitals and 84 outpatient clinics between 2000 and 2011. Of these, 16,216 patients with HFPEF (ejection fraction ≥40%; mean [SD] age, 75 [11] years; 46% women) were either treated (n = 12,543) or not treated (n = 3673) with RAS antagonists. Propensity scores for RAS antagonist use were derived from 43 variables. The association between use of RAS antagonists and all-cause mortality was assessed in a cohort matched 1:1 based on age and propensity score and in the overall cohort with adjustment for propensity score as a continuous covariate. To assess consistency, separate age and propensity score-matched analyses were performed according to RAS antagonist dose in patients with HFPEF and in 20,111 patients with HFREF (ejection fraction <40%) in the same registry.
Main outcome measure:
All-cause mortality.
Results:
In the matched HFPEF cohort, 1-year survival was 77% (95% CI, 75%-78%) for treated patients vs 72% (95% CI, 70%-73%) for untreated patients, with a hazard ratio (HR) of 0.91 (95% CI, 0.85-0.98; P = .008). In the overall HFPEF cohort, crude 1-year survival was 86% (95% CI, 86%-87%) for treated patients vs 69% (95% CI, 68%-71%) for untreated patients, with a propensity score-adjusted HR of 0.90 (95% CI, 0.85-0.96; P = .001). In the HFPEF dose analysis, the HR was 0.85 (95% CI, 0.78-0.83) for 50% or greater of target dose vs no treatment (P < .001) and 0.94 (95% CI, 0.87-1.02) for less than 50% of target dose vs no treatment (P = .14). In the age and propensity score-matched HFREF analysis, the HR was 0.80 (95% CI, 0.74-0.86; P < .001).
Conclusion:
Among patients with heart failure and preserved ejection fraction, the use of RAS antagonists was associated with lower all-cause mortality.
Facebook Comments