ReachMD
Be part of the knowledge.™Short time to furosemide treatment increases survival in acute heart failure
Background
Recent heart failure (HF) guidelines emphasize the importance of the immediate diagnosis and treatment of patients presenting with acute HF (AHF) in the emergency department (ED). This is based on retrospective data showing that the efficacy of any intervention/treatment may be time-dependent in this setting [1-5].
In current analysis of the multi-center REALITY-AHF registry, the association between time to treatment and clinical outcomes was prospectively evaluated in patients with AHF presenting at the ED. In this way the prognostic impact of time to treatment for AHF performed in the acute phase was determined.
The AHF diagnosis was based on the Framingham criteria. The following patients were excluded: patients who received IV treatment before their arrival at the ED, those with a previous heart transplantation, or on chronic peritoneal dialysis or hemodialysis, or with acute myocarditis, or ACS requiring PCI, as well as patients without BNP or NT-proBNP data or with a BNP level<100 pg/ml or a NT-proBNP level <300 pg/ml at baseline.
The primary pre-specified variable was the door-to-furosemide (D2F) time, defined as the time from ED arrival to the “first IV furosemide” administration. Patients were divided into the early and the non-early treatment groups, using a cutoff of 60 minutes. The primary endpoint was all-cause in-hospital mortality.
Main results
- Out of 1,291 eligible patients, 481 patients (37.3%) were in the early treatment group and 810 (62.7%) in the non-early treatment group. The median D2F time was 90 minutes (IR: 36-186 minutes).
- Arriving by ambulance and the presence of signs and symptoms of congestion, including orthopnea, jugular venous distension, ARB prescription at admission and a high heart rate, were independently associated with a shorter D2F time.
- The early treatment group had a slightly lower GWTG-HF risk score than the non-early treatment group.
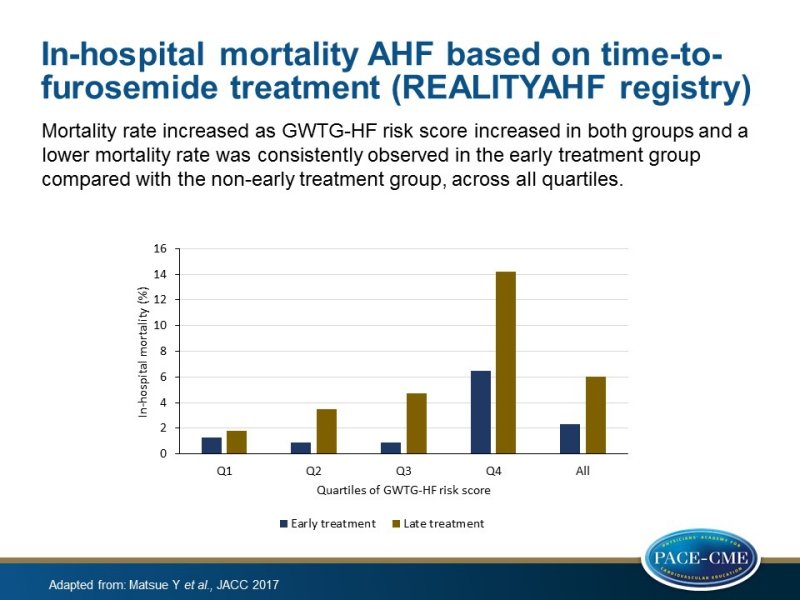
- Although the mortality rate increased as GWTG-HF risk score increased in both groups (P for trend <0.05 for both groups), a lower mortality rate was consistently observed in the early treatment group compared with the non-early treatment group across all quartiles, with the absolute risk difference increasing as the Get With the Guidelines-Heart Failure risk score (GWTG-HF, based on race, age, systolic blood pressure, heart rate, blood urea nitrogen, sodium levels, and the presence of chronic obstructive pulmonary disease) quartile rose (P for trend=0.027).
- Early treatment was associated with lower in-hospital mortality in univariate analysis (OR: 0.36; 95% CI: 0.21 - 0.62; P<0.001) and after adjustment for the GWTG-HF risk score (OR: 0.42; 95% CI: 0.24 -0.72; P<0.001).
- In multivariable analysis, no significant interaction was seen between the early treatment group and the GWTG-HF risk score on in-hospital mortality (P for interaction=0.916), nor with any of the congestion symptoms, arrival with or without ambulance or gender (P for interaction >0.3 for all).
- The association between early treatment and in-hospital mortality did not differ significantly in patients with a history of HF (OR: 0.43; 95% CI: 0.19 - 1.00; P=0.051) and without a history of HF (OR: 0.34; 95% CI: 0.11 - 1.03; P=0.057) (P for interaction=0.738).
- In sensitivity analyses, the association between log D2F time and in-hospital mortality remained statistically significant (OR: 1.31; 95% CI: 1.04 - 1.64; P=0.021 for the logistic regression model and OR: 1.31; 95% CI: 1.01 - 1.71; P=0.045 for the GEE [generalized estimating equation] model).
- In the propensity score analysis, 708 patients were matched based on the propensity score. In-hospital mortality was, once again, lower in the early treatment group compared with that in the non-early treatment group (5.9% vs. 2.5%; P=0.038; OR: 0.41; 95% CI: 0.18 - 0.89; P=0.030).
Conclusion
In a prospective observational study, patients with AHF presenting at the ED with severe congestive symptoms were more likely to be treated early with IV furosemide, and treatment with IV furosemide within 60 min was independently associated with a better in-hospital survival.
References
1. Mebazaa A, Pang PS, Tavares M, et al. The impact of early standard therapy on dyspnoea in patients with acute heart failure: the URGENT dyspnoea study. Eur Heart J 2010;31:832–41.
2. Maisel AS, Peacock WF, McMullin N, et al. Timing of immunoreactive B-type natriuretic peptide levels and treatment delay in acute decompensated heart failure: an ADHERE (Acute Decompensated Heart Failure National Registry) analysis. J Am Coll Cardiol 2008;52:534–40.
3. Peacock WF, Emerman C, Costanzo MR, et al. Early vasoactive drugs improve heart failure outcomes. Congest Heart Fail 2009;15:256–64.
4. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur J Heart Fail 2016;18:891–975.
5. Mebazaa A, Yilmaz MB, Levy P, et al. Recommendations on pre-hospital & early hospital management of acute heart failure: a consensus paper from the Heart Failure Association of the European Society of Cardiology, the European Society of Emergency Medicine and the Society of Academic Emergency Medicine. Eur J Heart Fail 2015;17:544–58.
Facebook Comments