ReachMD
Be part of the knowledge.™NP-guided treatment reduced all-cause mortality in patients with chronic HF <75 years old
Troughton RW, Frampton CM, Brunner-La Rocca HP, et al.
Eur Heart J. 2014 Mar 6. [Epub ahead of print]
Background
It is a topic of debate how to best guide the complex pharmacotherapy of chronic heart failure (CHF). While it has been shown that survival of patients with CHF and reduced left ventricular ejection fraction (LVEF) can be improved with angiotensin converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARBs), certain beta-blockers (BB) and mineralocorticoid receptor antagonists (MRAs) [1], optimal dosing is largely guided by subjective indices. As a result, evidence-based target doses of these medications are rarely achieved outside the trial setting [2].It would be helpful if pharmacotherapy could be guided by an objective index of circulatory status. B-type cardiac natriuretic peptides (BNP and NT-proBNP), which are released from the heart in proportion to stretch of the cardiac chambers, have been proposed to be such a guide. Indeed, levels of these peptides over time provide a robust prognostic index in CHF [3]. Also, drugs that have been shown to increase survival reduce the levels of natriuretic peptides [4].
Published evidence to date is insufficient to support routine NP-guided treatment, due to lack of adequate power in studies evaluating the effect on all-cause mortality. This is an individual patient data meta-analysis to test the hypothesis that NP-guided therapy leads to lower all-cause mortality as compared with conventional clinically guided management. A total of 8 studies met all eligibility criteria, amounting to individual patient data of 2000 cases for all-cause mortality.
Main results
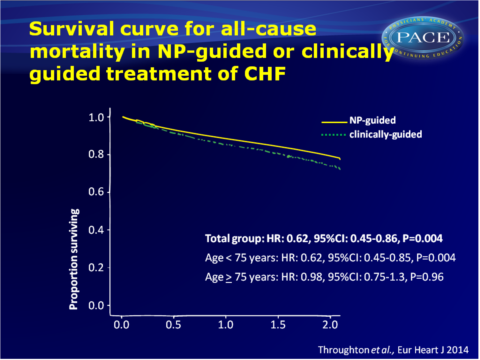
- During active treatment, 207 patients deceased assigned to clinically guided treatment, as compared with 172 deaths in the NP-guided group (HR: 0.62, 95%CI: 0.45-0.86, P=0.004). There was no significant heterogeneity between the studies.
- Age significantly affected treatment efficacy, in that a survival benefit was seen for NP-guided vs. clinically guided treatment in patients younger than 75 years old (HR: 0.62, 95%CI: 0.45-0.85, P=0.004), but not in patients older than 75 (HR: 0.98, 95%CI: 0.75-1.03, P=0.96).
No interaction was seen between LVEF and the relationship between treatment and all-cause mortality. - As secondary endpoints, HF hospitalisations were reduced in the NP-guided group (n=247 vs. n-294, HR: 0.80, 95%CI: 0.67-0.94, P=0.009), as well as cardiovascular admissions (n=430 vs. n=448, HR: -.82, 95%CI: 0.67-0.99, P=0.048). There was no heterogeneity between studies and no interactions were seen for age or LVEF.
- Follow-up plasma NT-proBNP levels were available of 1313 participants. A similar fall in NT-proBNP levels was seen in the NP-guided group (35.0%, 95%CI: 28.5-41.0) and in the clinically guided group (31.5%, 95%CI: 24.5-37.8, P=0.44). The fall in NT-proBNP levels was larger in patients younger than 75 years, but to a similar extent in both treatment groups.
- At the end of follow-up, ACEi/ARB dosing had increased in the NP-guided group (+8.4%, 95%CI: 3.4-13.5 enapralil equivalents), while it had changed little in the clinically guided group (-1.2%, 95%CI: -6.1% to 3.7%, P=0.007 for group comparison). There was a strong age interaction, with an increase in ACEi/ARB dosing in patients younger than 75 in both treatment groups (although a larger increase in NP-guided patients), and a decrease in patients older than 75 in the control group.
- Increasing dose of ACEi/ARB, BB and MRA were each significantly associated with reduced all-cause mortality.
Download Throughton EHJ 2014 pace.pptx
Conclusion
This study supports the hypothesis that circulating levels of B-type natriuretic peptides can provide an objective index of circulatory status in patients with CHF, and can thereby allow clinicians to more accurately target pharmacotherapy to the individual patient. The authors believe that these data should lead to reconsideration of the currently rather cautious clinical recommendations of specialist societies.For CHF patients younger than 75, most of whom had impaired LVEF, NP-guided treatment reduced all-cause mortality, as compared with clinically guided therapy. The NP-guided strategy also reduced hospitalisation for HF and CV disorders, irrespective of age. A large-scale, well-powered, randomised and blinded study could provide reassurance.
References
1. McMurray JJ, Adamopoulos S, Anker SD,et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012;33:1787–1847.
2. Lenzen MJ, Boersma E, Scholte op Reimer WJM, et al. Under- utilization of evidence-based drug treatment in patients with heart failure is only par- tially explained by dissimilarity to patients enrolled in landmark trials: a report from the Euro Heart Survey on Heart Failure. Eur Heart J 2005;26:2706 – 2713.
3. MassonS, Latini R, AnandI S, et al. Prognostic value of changes in N-terminal pro-brain natriuretic peptide in Val-HeFT (Val- sartan Heart Failure Trial). J Am Coll Cardiol 2008;52:997–1003.
4. Troughton RW, Richards AM, Yandle TG, et al.The effects of medications on circulating levels of cardiac natriuretic peptides. Ann Med 2007;39: 242 – 260.
Find this article on Pubmed
Facebook Comments