ReachMD
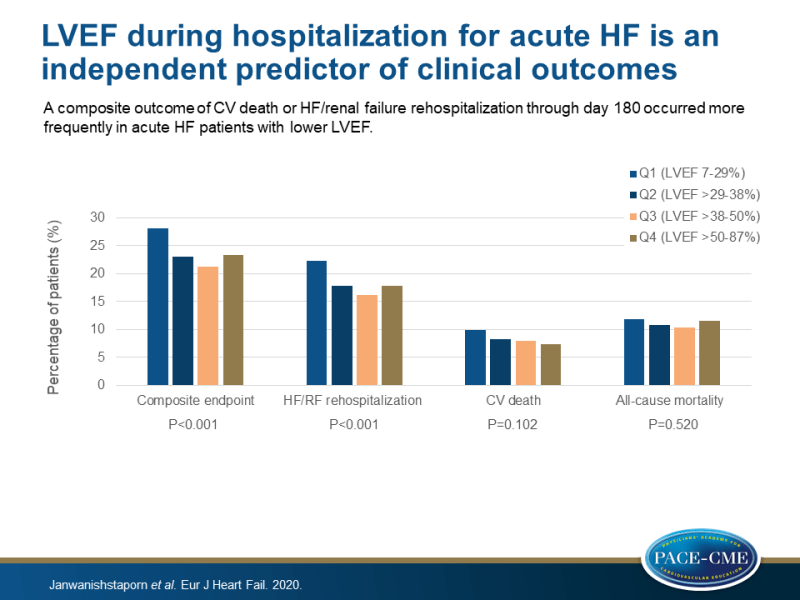
Be part of the knowledge.™LVEF during hospitalization for acute HF is an independent predictor of clinical outcomes
Introduction and methods
Hospitalization for acute HF (AHF) is a predictor for rehospitalization and CV mortality in the months after discharge [1]. However, this risk differs among HF patients, due to heterogeneity of the HF population. Information about the magnitude of risk in a patient with AHF following hospitalization is of importance in guiding the direction of medical management [2-4]. Left ventricular ejection fraction (LVEF) has been proven useful in confirming the diagnosis of HF and in setting recommendations for medical therapies [5]. However, the value of LVEF in predicting the clinical outcome of patients with AHF after hospitalization is unclear. This study evaluated the relationship between LVEF measured during AHF hospitalization and outcomes after discharge in the Relaxin in Acute Heart Failure 2 (RELAX-AHF-2) trial.
The RELAX-AHF-2 was a multicenter, randomized, double-blind, placebo-controlled phase 3 trial that enrolled hospitalized patients with AHF [6]. Patients were randomized to receive either serelaxin for 48h or matching placebo. The two treatment arms were pooled in the present analyses, because of the neutral effect of serelaxin on the studied outcomes, consisting of CV death and worsening HF [7]. 6128 Patients were included in the present analyses. Patients were classified based on LVEF measured during index hospitalization: Q1, LVEF 17-29% (n=1548); Q2, LVEF >29-38% (n=1556); Q3, LVEF >38-50% (n=1815); and Q4, LVEF >50-87% (n=1209). LVEF was also analyzed as a continuous variable.
The primary composite endpoint was CV death or HF/renal failure (RF) rehospitalization through day 180. Other outcomes were the two components of the composite outcome separately and all-cause mortality through day 180.
Main results
- For the primary composite endpoint, significant differences between quartiles were found with the highest rate in quartile 1 patients (28.2% in Q1 vs. 23.3% in Q4, P<0.001). Significant differences between quartiles were also found for HF/RF rehospitalization through 180 days (22.3% in Q1 vs. 17.8% in Q4, P<0.001), but not for either CV or all-cause mortality.
- Each 5% increase in LVEF associated with significant reduction in the risk for the composite endpoint (adjusted HR 0.97, 95%CI 0.94–0.99; P=0.009) and for HF/RF rehospitalization at day 180 (adjusted HR 0.95, 95%CI 0.93–0.98; P<0.001).
- Using smooth spline modelling, risk for the composite outcome remained stable as LVEF decreases until it reaches a value of approximately 40%. Below this LVEF value, the risk progressively increased. A similar pattern was found for HF/RF rehospitalization. No significant association between LVEF and all-cause mortality was found.
- Patients with an ischemic etiology had a higher risk for the composite outcome compared with those with a non-ischemic etiology. A significant difference was observed in the composite outcome across LVEF quartiles in patients with an ischemic etiology (P<0.0001 by log-rank test). This was less robust in patients with a non-ischemic etiology (P=0.039) (P-interaction=0.019). Also, risk for the composite endpoint was greater in patients with lower LVEF whose index event was due to decompensation of existing HF (P<0.0001 by log-rank test), but not in patients with de novo HF (P-interaction 0.047).
Conclusion
In patients hospitalized with AHF, the composite outcome of CV death or HF/RF rehospitalization through day 180 occurred significantly more frequently in patients in the lowest LVEF quartile compared to those in the highest quartile. This result was predominantly driven by the higher risk of HF/RF rehospitalization. The risk of the composite outcome and HF/RF rehospitalization progressively increased as LVEF was reduced below 40%.
References
1. Go YY, Sellmair R, Allen JC Jr, Sahlen A, Bulluck H, Sim D, Jaufeerally FR, MacDonald MR, Lim ZY, Chai P, Loh SY, Yap J, Lam CS. Defining a ‘frequent admitter’ phenotype among patients with repeat heart failure admissions. Eur J Heart Fail 2019;21:311–318.
2. Miro O, Rossello X, Gil V, Martin-Sanchez FJ, Llorens P, Herrero-Puente P, Jacob J, Bueno H, Pocock SJ. Predicting 30-day mortality for patients with acute heart failure in the emergency department: a cohort study. Ann Intern Med 2017;167:698–705.
3. Peterson PN, Rumsfeld JS, Liang L, Albert NM, Hernandez AF, Peterson ED, Fonarow GC, Masoudi FA. A validated risk score for in-hospital mortality in patients with heart failure from the American Heart Association Get With the Guidelines program. Circ Cardiovasc Qual Outcomes 2010;3:25–32.
4. Lee DS, Lee JS, Schull MJ, Borgundvaag B, Edmonds ML, Ivankovic M, McLeod SL, Dreyer JF, Sabbah S, Levy PD, O’Neill T, Chong A, Stukel TA, Austin PC, Tu JV. Prospective validation of the Emergency Heart Failure Mortality Risk Grade for acute heart failure. Circulation 2019;139:1146–1156.
5. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2016;18:891–975.
6. Teerlink JR, Voors AA, Ponikowski P, Pang PS, Greenberg BH, Filippatos G, Felker GM, Davison BA, Cotter G, Gimpelewicz C, Boer-Martins L,Wernsing M, Hua TA, Severin T, Metra M. Serelaxin in addition to standard therapy in acute heart failure: rationale and design of the RELAX-AHF-2 study. Eur J Heart Fail 2017;19:800–809.
7. Metra M, Teerlink JR, Cotter G, Davison BA, Felker GM, Filippatos G, Greenberg BH, Pang PS, Ponikowski P, Voors AA, Adams KF, Anker SD, Arias-Mendoza A, Avendaño P, Bacal F, Böhm M, Bortman G, Cleland JGF, Cohen-Solal A, Crespo-Leiro MG, Dorobantu M, Echeverría LE, Ferrari R, Goland S, Goncalvesová E, Goudev A, Køber L, Lema-Osores J, Levy PD, McDonald K, Manga P, Merkely B, Mueller C, Pieske B, Silva-Cardoso J, Špinar J, Squire I, Stepinska J, Van Mieghem W, von Lewinski D, Wikström G, Yilmaz MB, Hagner N, Holbro T, Hua TA, Sabarwal SV, Severin T, Szecsödy P, Gimpelewicz C; RELAX-AHF-2 Committees and Investigators. Effects of serelaxin in patients with acute heart failure. N Engl J Med 2019;381:716–726.
Facebook Comments