ReachMD
Be part of the knowledge.™HF with recovered ejection fraction has better, but not normal, prognosis than HF-PEF and HF-REF
Basuray A, French B, Ky B et al.
Circulation. 2014 Jun 10;129(23):2380-7
Background
The primary goal of therapy in heart failure (HF) with reduced ejection fraction (HF-REF) is recovery of left ventricular (LV) function. Little is known about the natural history, prognosis, and need for continued long-term therapies in patients in the case of recovery of LV function [1-4]. Some of the patients with HF and recovered ejection fraction (HR-Recovered) may continue HF-REF treatment, while others may discontinue therapy, or be wrongly classified as having HF with preserved ejection fraction (HF-PEF) [5].Reverse remodelling or myocardial remission, towards better EF, in response to therapy may result in a milder HF phenotype and a better prognosis [6].
This study aimed to characterize the HF-Recovered population, and compare these patients with those with HF-REF and HF-PEF. Data of 1821 patients of the Penn Heart Failure Study cohort were used, of whom 1523 had HF-REF (mean EF: 27%), 122 had HF-PEF (mean EF: 62%) and 176 patients had HF-Recovered (mean EF: 57%). Patients were followed up for a median of 3.6 years, with a maximum of 8.9 years.
Main results
- HF-Recovered patients had less severe symptoms (more patients in New York Heart Association class I or II) than HF-REF or HF-PEF patients. HF-Recovered and HF-REF patients received beta-blockers or ACE-inhibitors or ARBs more often than HF-PEF patients. Aldosterone antagonists, digoxin and diuretics were most often used in patients with HF-REF.
- Mean blood pressure was higher in the HF-Recovered group than in HF-REF, but lower than in HF-PEF patients. No differences were seen for mean serum sodium levels.
- 30% of HF-Recovered patients still had a BNP level above the 95th percentile (135 pg/mL). 47% of HF-Recovered patients had uric acid levels above the 95th percentile (2.6-6 mg/dL for women and 3.5-7.2 mg/dL for men). Detectable troponin I levels were seen in 44% of HF-Recovered patients.
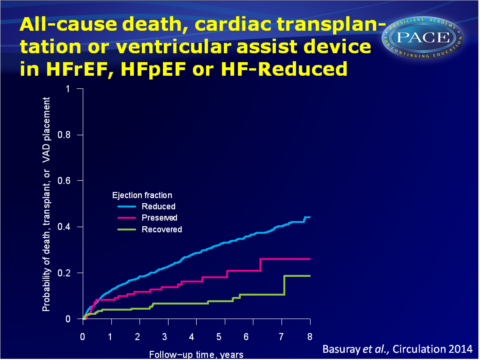
- In unadjusted Cox models, HR for all-cause death, cardiac transplantation or ventricular assist devices (VADs) placement in the HF-REF vs. the HF-Recovered group was 4.1 (95%CI: 2.4-6.8, P<0.001). HR for HF-PEF vs. HF-Recovered was 2.3 (95%CI: 1.2-4.5, P=0.013). These associations remained statistically significant in multivariable-adjusted models. Nearly 20% of the HF-Recovered population suffered from death, cardiac transplantation or VAD placement by 8 years of follow-up.
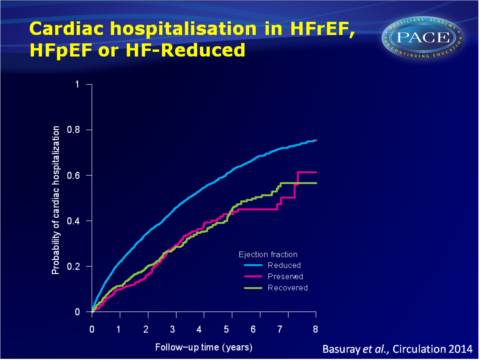
- HF-Recovered patients had a number of hospitalisations similar to that in HF-PEF patients. In recurrent event-models, no statistically significant difference in cardiac hospitalisations was seen between HF-PEF and HF-Recovered (HR: 1.3, 95%CI: 0.90-2.0). The unadjusted HR for HF-REF vs. HF-Recovered was 2.0 (95%CI: 1.5-2.7, P<0.001), which remained significant after correction for potential confounders.
- Despite better clinical and biochemical profile at baseline and event-free survival than HF-REF patients, HF-Recovered patients remain at risk for adverse events, since part of the patients show abnormal biomarker levels and the hospitalisation rates are similar to those of HF-PEF patients.
Download Basuray circulation 2014 PACE.pptx
Conclusion
These data suggest that HF-Recovered represents a distinct phenotype on the HF continuum, since this population has different demographics, comorbidities and symptom severity from HF-REF and HF-PEF populations. HF-Recovered patients may have abnormal BNP, uric acid, ST2, SFlt-1 and detectable troponin I, suggestive of persistent neurohormonal activation, increased oxidative stress and cardiomyocyte injury and stress, despite recovery of EF. Although HF-Recovered patients had the best prognosis with regard to death, cardiac transplantation and VAD placement, it is not at all a normal prognosis, as HF symptoms and clinical events continue to occur. Thus, recovery of EF does not necessarily mean recovery of HF. Further pathophysiological characterisation should help to better tailor therapy in these patients.Editorial comment [7]
This study provides valuable characterisation of the population in whom LV EF has improved to >0.50. These patients should indeed not be classified as HF-PEF, and initiation or investigation of therapies intended for HF with low EF should be discouraged without confirmation that EF remains low.Despite EF>0.50, convincing clinical and biochemical evidence was presented that heart dysfunction has not truly recovered in these patients. It is proposed to call this condition HF better EF. Further characterisation of these patients will reveal how many patients have multiple abnormalities and whether patients exist who have entirely normalised profiles. The population with HF and low, improving EF has been recognised as a distinct population in the last American College of Cardiology Foundation/American Heart Association guidelines [8].”The delineation of HF better EF is 1 example of an important new diagnosis arising and defined from our recent therapies. Collaborative clinical and molecular scrutiny of this modern population will catalyze new insight into fundamental questions of how HF recompensates and what can truly recover, and ultimately help us to support and sustain recovery for patients with HF.”
Find this article on Pubmed
References
1. Steimle AE, Stevenson LW, Fonarow GC, et al. Prediction of improvement in recent onset cardiomyopathy after referral for heart transplantation. J Am Coll Cardiol. 1994;23:553–559.
2. Moon J, Ko YG, Chung N, et al. Recovery and recurrence of left ventricular systolic dysfunction in patients with idiopathic dilated cardiomyopathy. Can J Cardiol. 2009;25:e147–e150.
3. Teeter WA, Thibodeau JT, Rao K, et al. The natural history of new-onset heart failure with a
severely depressed left ventricular ejection fraction: implications for timing of implantable cardioverter-defibrillator implantation. Am Heart J. 2012;164:358–364.
4. McNamara DM, Starling RC, Cooper LT, et al; IMAC Investigators. Clinical and demographic predictors of outcomes in recent onset dilated cardiomyopathy: results of the IMAC (Intervention in Myocarditis and Acute Cardiomyopathy)-2 study. J Am Coll Cardiol. 2011;58:1112–1118.
5. Punnoose LR, Givertz MM, Lewis EF, et al. Heart failure with recovered ejection fraction: a distinct clinical entity. J Card Fail. 2011;17:527–532.
6. Mann DL, Barger PM, Burkhoff D. Myocardial recovery and the failing heart: myth, magic, or molecular target? J Am Coll Cardiol. 2012;60:2465–2472.
7. Stevenson LW. Heart Failure With Better Ejection Fraction: A Modern Diagnosis. Circulation. 2014;129:2364-2367
8. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:1810–1852.
Facebook Comments